You control your data
You control your data. You decide what is shared, with whom and when.
One place for your whole health.
Health, fitness & wellbeing for your whole family, in one simple app.
Connected care that works.
Bringing everything together so you don’t have to join the dots.
Free for the public and charities.
Access to trusted, evidence-based health support should be universal.
Trusted. Neutral. Connected
A platform designed for people, healthcare teams and partners across the ecosystem.
Our health systems are full of people who care. The real problem is the way everything fits together, not the people inside it.
Every day, across every setting, healthcare professionals do their best. They save lives, improve care and show up for us, our families and our communities.
But they are working inside a system that was never built as one connected whole.
Standards vary. Information gets lost. Progress moves more slowly than people need.
These are structural issues, not human ones. And the impact is felt most by the people the system is meant to help.
People wait, often for years. The path to diagnosis can be long and confusing, with repeated tests and appointments that never quite join up. Families carry the emotional and practical load. They try to make sense of a system that does not feel built for them.
This fragmentation affects professionals too. Many face burnout. They are asked to do more with less time, fewer resources and incomplete information.
Somewhere along the way, the system loses sight of what it exists to do. Help people.
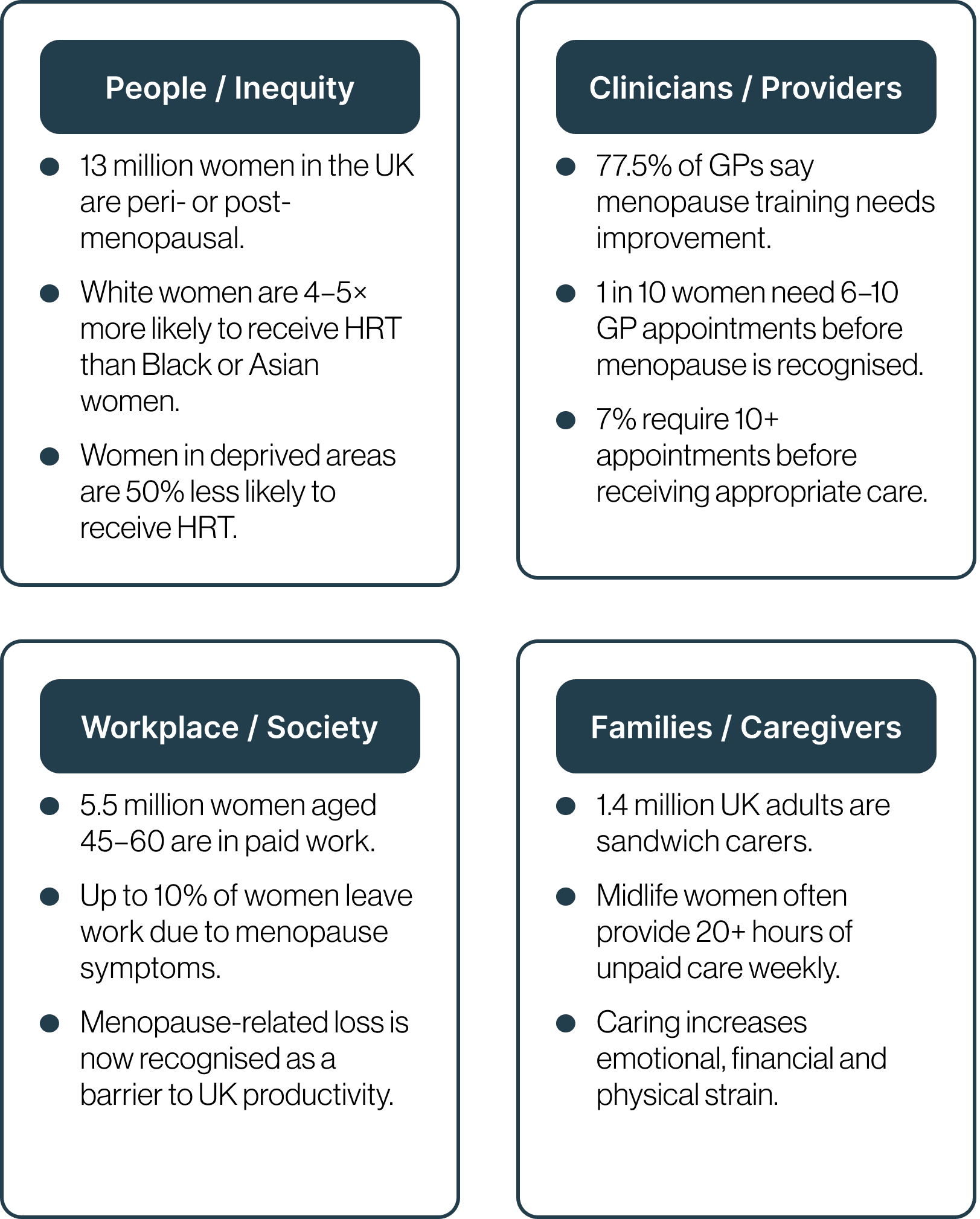
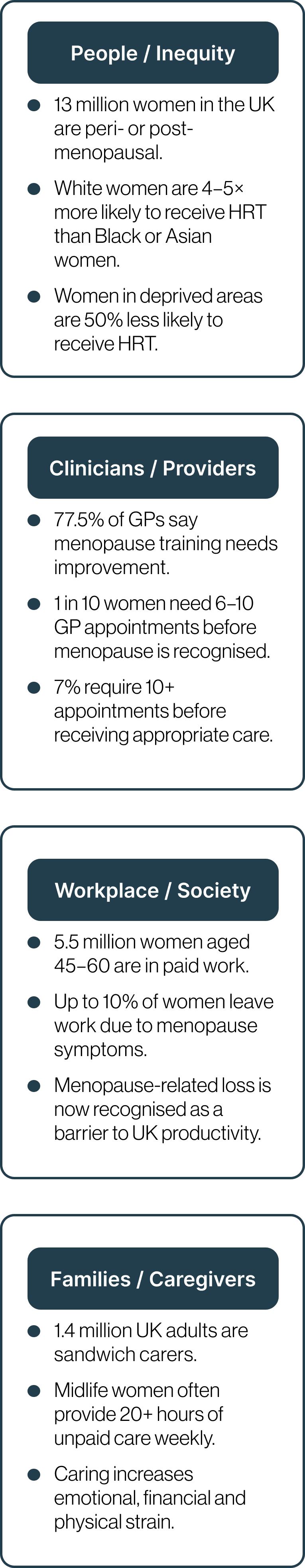
Across the UK, millions of women transition through perimenopause and menopause each year. Similar patterns are seen across Europe, North America and Asia. For many, this stage of life brings changes that can affect sleep, mood, memory, work and relationships — yet the journey to reliable support often feels slow and fragmented.
On average, women wait 7–8 years from the onset of symptoms to a diagnosis or meaningful help. Many speak to several clinicians, repeat their story again and again, and still feel unheard.
Three quarters of women experience symptoms, and around a quarter say those symptoms significantly disrupt daily life. But support varies widely. Women in deprived areas are less likely to receive timely care, and women from Black and Asian communities report lower access to evidence-based treatment and a higher likelihood of being dismissed or misdiagnosed.
This is not a story of individual failure. It is a system struggling to recognise patterns early, connect information consistently and support women with the clarity and compassion they deserve.
When early signals are missed, conditions grow silently.
More than 64 percent of adults in England are living with excess weight, and one in four adults meet the clinical definition of obesity. Similar or rising trends are found across the United States, Europe, the Middle East and Asia.
Excess weight is often the beginning of a cascade of metabolic risks. Type 2 diabetes, high blood pressure, fatty liver, cardiovascular disease and cognitive decline are all linked. As these risks build, health deteriorates quickly. Around 30 percent of adults with one chronic condition report poor health. This rises to more than 80 percent for those with three or more.
Yet these signals often go unnoticed. People are treated for individual symptoms, in individual appointments, across disconnected services. A system that treats the condition and not the human.
The result is predictable. More people enter the system in poorer health, needing more complex support through pathways that were never designed to work together.
Clinicians feel this too. Nearly one third of NHS staff report burnout, and similar pressures are seen in health systems worldwide.
This is a global pattern. Rising excess weight. Rising metabolic disease. Rising multimorbidity. Rising strain.
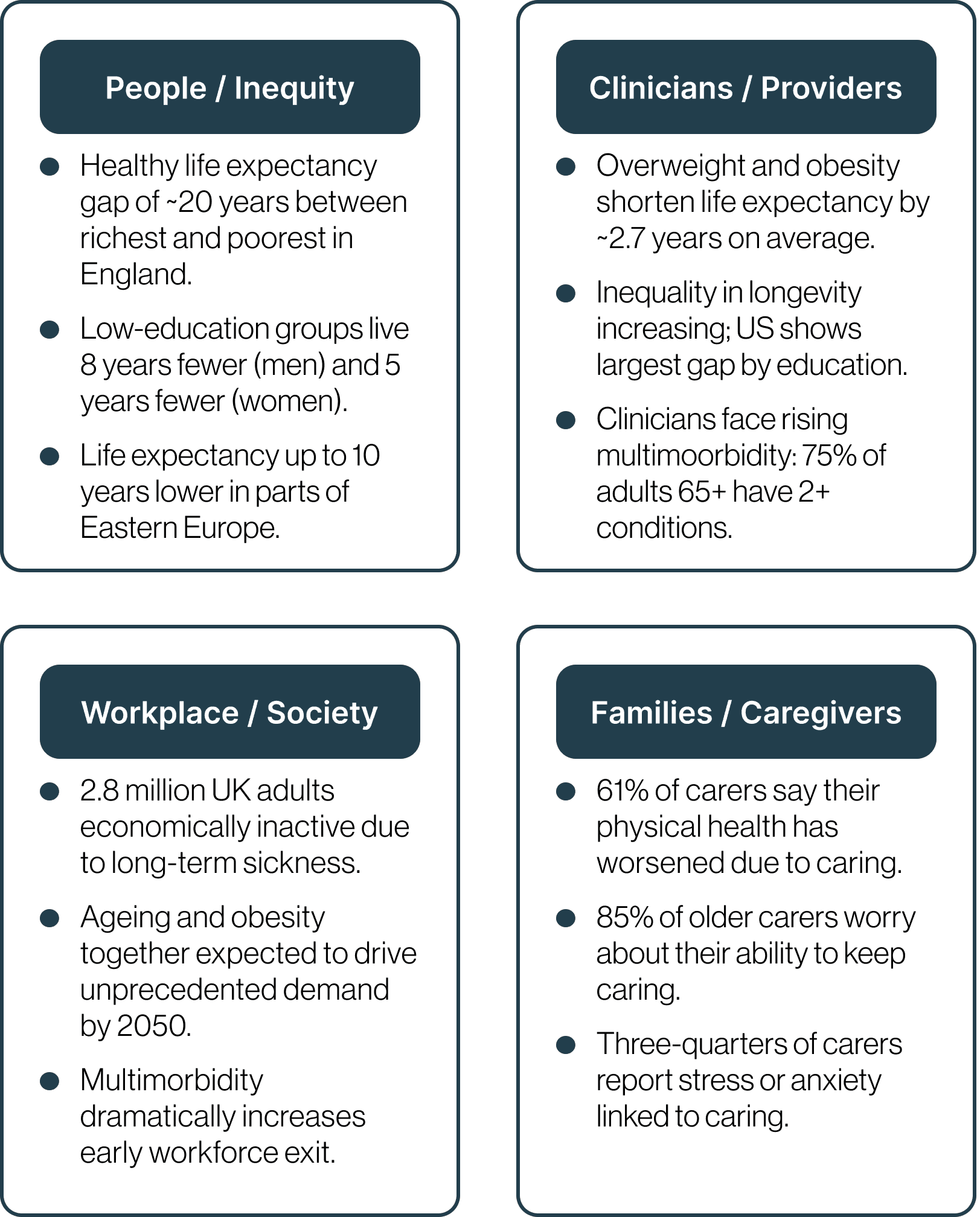
Living longer does not always mean living well.
Across England, the gap in healthy life expectancy is more than 19 years for men and more than 20 years for women. Globally, similar and growing gaps appear across Europe, the Gulf, Asia and North America.
Life expectancy is rising, but many people spend more years in poor health. More people enter mid life and later life with multiple unmanaged conditions. Metabolic risks, cardiovascular disease, mental health challenges, musculoskeletal pain and cognitive decline are all increasing.
Healthy life expectancy has stalled. In many places it is falling. This means more years lived in poor health, rising dependency and preventable complexity.
The strain is felt everywhere. Families take on more care. Workplaces lose experience. Communities age unevenly. Clinicians face rising multimorbidity with limited time and fragmented information. The system struggles because it was built for single conditions, not the interconnected reality of human health.
When early signals are missed and services are not joined up, people slip through the cracks for years and inequity widens.
The Bridge
GAiA Health is the bridge that connects people, professionals and partners a single space where information flows, journeys connect and decisions become clearer.
By linking prevention, daily health, care pathways and real-world experience, GAiA helps the system listen, learn and work as one.
Benefiting people at every point.
The Solution
More than a healthcare system. A healthcare experience designed around whole humans.
GAiA Health brings people, clinicians and partners together on one trusted platform so care feels connected, informed and designed around real lives.
People get clear, evidence-based information when they need it. Clinicians get time back and a fuller picture. Partners gain a shared foundation that reduces duplication and improves transparency.
A more connected way to care. A system that can finally see the whole human
Prevention. Access. Clarity. Impact.
Join people and healthcare teams who trust GAiA Health to make everyday health feel clearer, safer and more connected.